Hiatal hernia is a condition where part of the stomach pushes upward into the chest cavity through an opening in the diaphragm. While many people with this condition experience no symptoms, others may suffer from discomfort, acid reflux, or difficulty swallowing. When lifestyle changes and medication fail to relieve symptoms, Hiatal Hernia Surgery may be recommended. This surgery helps to repair the hernia and alleviate the symptoms that affect a person’s quality of life. In this article, we will explore what hiatal hernia surgery entails, the procedure, recovery, and when it’s necessary.
What Is Hiatal Hernia?
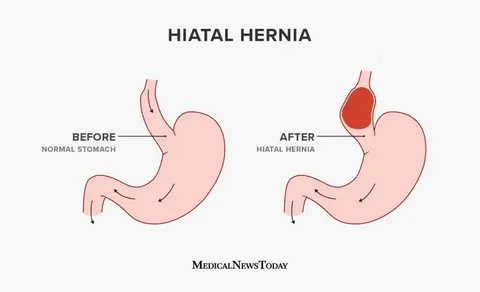
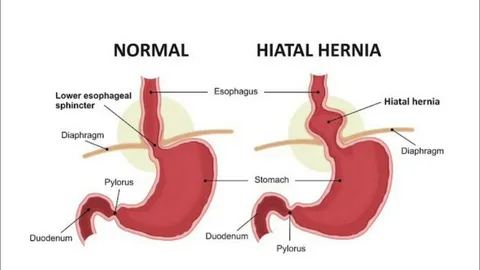
A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity. This condition often goes unnoticed and can remain asymptomatic for years. However, when symptoms such as heartburn, chest pain, difficulty swallowing, and regurgitation occur, medical intervention may be needed.
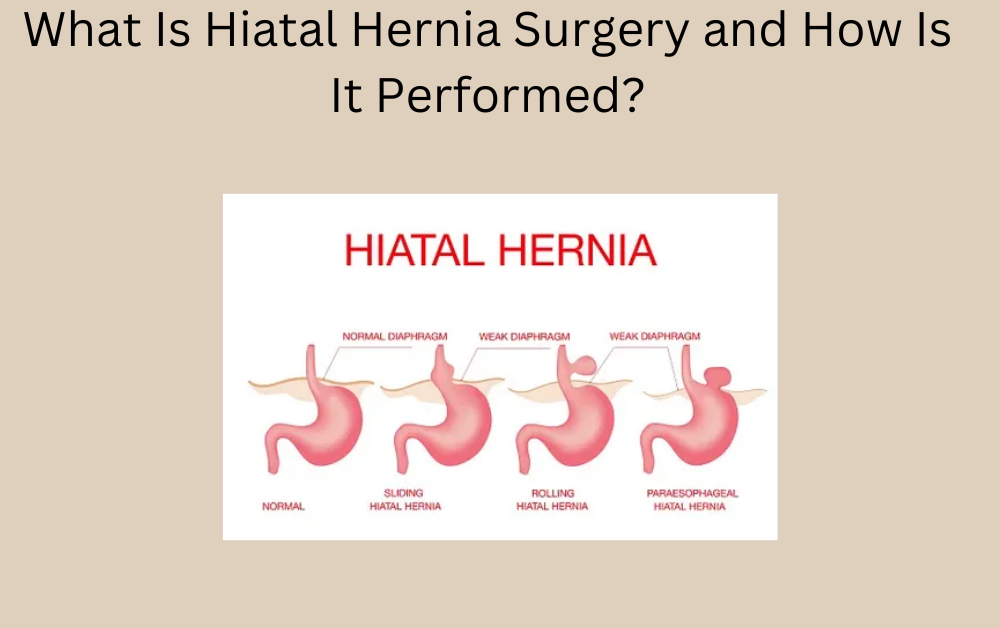
There are two main types of hiatal hernias: sliding and paraesophageal. The most common is the sliding hiatal hernia, where the stomach and part of the esophagus slide up into the chest through the diaphragm. A paraesophageal hernia, though less common, occurs when part of the stomach pushes through the diaphragm next to the esophagus, potentially leading to more severe complications.
Note: Hiatal Hernia Surgery in Dubai performed by Dr. Dameh helped many patients find relief from painful symptoms. With his skilled approach, patients were able to heal quickly and return to daily activities. Reach out to Dr. Dameh now for expert care and treatment for your condition.
When Is Hiatal Hernia Surgery Necessary?
While many individuals with a hiatal hernia can manage their symptoms with dietary changes, medications, and lifestyle adjustments, surgery may become necessary if symptoms are severe, persistent, or if complications arise. If a hernia is causing frequent acid reflux, bleeding, or other complications, surgical intervention can help reduce the risk of further damage.
Hiatal hernia surgery may also be recommended for those who experience:
- Severe gastroesophageal reflux disease (GERD) that doesn’t respond to medications
- Difficulty swallowing (dysphagia) due to the hernia
- Severe chest pain or discomfort caused by the hernia
- A paraesophageal hernia that may result in strangulation of the stomach
In these cases, surgery aims to repair the hernia and restore normal function, improving quality of life.
Types of Hiatal Hernia Surgery
There are several surgical methods to treat a hiatal hernia, each varying in approach and complexity. The type of surgery recommended depends on the size of the hernia, the symptoms, and any existing complications. Here are the most common types of hiatal hernia surgery:
Laparoscopic Hiatal Hernia Surgery
Laparoscopic surgery, also known as minimally invasive surgery, is the most commonly performed method to treat hiatal hernia. During this procedure, the surgeon makes small incisions in the abdomen through which a camera and surgical instruments are inserted. The surgeon then repairs the hernia, typically by pulling the stomach back into place and tightening the opening in the diaphragm to prevent further herniation.
This method offers several benefits, including a shorter recovery time, less pain, and minimal scarring. It also reduces the risk of infection compared to open surgery. Laparoscopic surgery is generally suitable for most patients with hiatal hernias.
Open Hiatal Hernia Surgery
In some cases, open surgery may be necessary, especially when the hernia is large or has caused significant complications. Open surgery involves making a larger incision in the abdomen to access the hernia directly. The surgeon will then reposition the stomach and repair the diaphragm.
While open surgery can be effective, it comes with a longer recovery period, increased risk of infection, and more noticeable scarring compared to laparoscopic surgery. It is typically only recommended when laparoscopic surgery is not possible or if the hernia is difficult to repair.
Fundoplication
Fundoplication is often performed alongside laparoscopic or open surgery to treat acid reflux, a common symptom of a hiatal hernia. In this procedure, the top of the stomach is wrapped around the lower esophagus to prevent stomach acid from rising into the esophagus, thus preventing acid reflux. This procedure can be performed at the same time as the hernia repair or as a separate treatment for GERD.
Preparing for Hiatal Hernia Surgery
Before undergoing hiatal hernia surgery, patients are thoroughly evaluated to determine the best approach based on their condition. This may include:
- Medical History and Physical Exam: The surgeon will review your medical history, perform a physical examination, and assess any symptoms you are experiencing.
- Imaging Tests: X-rays, CT scans, or endoscopy may be ordered to assess the size and type of the hernia and evaluate other underlying conditions.
- Blood Tests: These tests help to assess your overall health and ensure that you are fit for surgery.
Patients will also be advised to fast before surgery and follow any instructions provided by their healthcare provider, including stopping certain medications to reduce the risk of complications.
Recovery from Hiatal Hernia Surgery
After surgery, recovery typically involves a hospital stay of 1–2 days, depending on the procedure and individual circumstances. During recovery, patients are monitored for any complications, and pain is managed with medications.
- Postoperative Care: The first few weeks after surgery involve rest and gradual reintroduction of normal activities. Patients are usually advised to avoid heavy lifting and strenuous activity for several weeks.
- Dietary Modifications: Following surgery, patients may need to adhere to a soft-food diet and gradually return to solid foods as the digestive system heals.
- Follow-up Visits: Regular follow-up appointments with the surgeon are crucial to ensure that the surgery was successful and to monitor for any signs of complications.
Most patients experience significant relief from symptoms after recovery and are able to return to their normal activities with few restrictions. However, a small number of patients may require further treatment if complications arise.
Potential Risks and Complications
As with any surgery, hiatal hernia surgery carries certain risks. These include:
- Infection at the surgical site
- Bleeding or blood clots
- Difficulty swallowing (dysphagia)
- Recurrence of the hernia
- Injury to surrounding organs such as the spleen or liver
However, with appropriate care and a skilled surgeon, the risk of complications is minimized, and most patients experience significant improvement in their symptoms.
Conclusion
Hiatal hernia surgery is an effective treatment option for individuals who suffer from severe or persistent symptoms related to their hernia. Whether through laparoscopic or open surgery, the goal is to repair the hernia, alleviate symptoms such as acid reflux, and improve the patient’s quality of life. If you are experiencing symptoms that may be related to a hiatal hernia, consult with a specialist to determine the best treatment options for your condition.
For More Insightful Articles Related To This Topic, Feel Free To Visit: coknews