Benign Prostatic Hyperplasia (BPH), commonly known as prostate enlargement, is a condition that affects millions of men worldwide, particularly as they age. It can lead to a variety of urinary symptoms that significantly impact quality of life. While medications have been the first line of treatment, some patients may require more invasive interventions. Two primary options are Prostate Artery Embolization (PAE) and traditional surgical procedures. This article aims to explore both treatment options in detail, comparing their mechanisms, benefits, risks, and helping you determine which might be the right choice for you.
Understanding Benign Prostatic Hyperplasia (BPH)
Before diving into the treatment options, it’s crucial to understand what BPH is and how it affects men. The prostate is a gland that surrounds the urethra, the tube through which urine exits the body. As men age, hormonal changes can cause the prostate to enlarge, leading to symptoms such as:
- Frequent urination, especially at night (nocturia)
- Difficulty starting or maintaining urine flow
- Weak urine stream
- Incomplete bladder emptying
- Urgency to urinate
BPH is not cancerous and does not increase the risk of prostate cancer, but it can significantly impact a man’s quality of life, leading to discomfort and even anxiety.
Traditional Surgical Options for BPH
1. Transurethral Resection of the Prostate (TURP)
TURP is one of the most common surgical procedures for BPH. In this procedure:
- How it Works: The surgeon removes excess prostate tissue using a special instrument called a resectoscope, inserted through the urethra.
- Procedure Duration: The surgery typically takes about 60-90 minutes.
- Recovery: Patients usually stay in the hospital for 1-2 days and may have a catheter in place for several days post-surgery.
- Effectiveness: Studies show that TURP can effectively relieve symptoms in approximately 80-90% of patients.
Benefits of TURP:
- Proven effectiveness in symptom relief
- Short recovery period compared to open surgery
- Immediate improvement in urinary flow
Risks of TURP:
- Bleeding
- Infection
- Urinary incontinence
- Erectile dysfunction
- Retrograde ejaculation (where semen enters the bladder instead of exiting through the penis)
2. Laser Therapy
Laser surgery involves using laser energy to vaporize or cut away prostate tissue. There are several types of laser procedures, including:
- Holmium Laser Enucleation of the Prostate (HoLEP)
- Photoselective Vaporization of the Prostate (PVP)
How it Works:
- A laser fiber is inserted through the urethra, where it emits high-energy light to remove excess prostate tissue.
- The procedure can be performed under general or local anesthesia.
Benefits of Laser Therapy:
- Minimal bleeding
- Shorter catheterization time
- Reduced hospital stay
- Effective symptom relief
Risks of Laser Therapy:
- Similar to those of TURP, including bleeding, infection, and potential sexual side effects.
3. Open Prostatectomy
In cases of severely enlarged prostates, a more invasive approach may be needed, known as open prostatectomy.
How it Works:
- The surgeon makes an incision in the lower abdomen to remove prostate tissue directly.
- This is typically done under general anesthesia.
Benefits:
- Effective for significantly enlarged prostates.
- Offers immediate and significant symptom relief.
Risks:
- Longer recovery time
- Increased risk of complications, including bleeding and infection
- More significant postoperative pain
Prostate Artery Embolization (PAE)
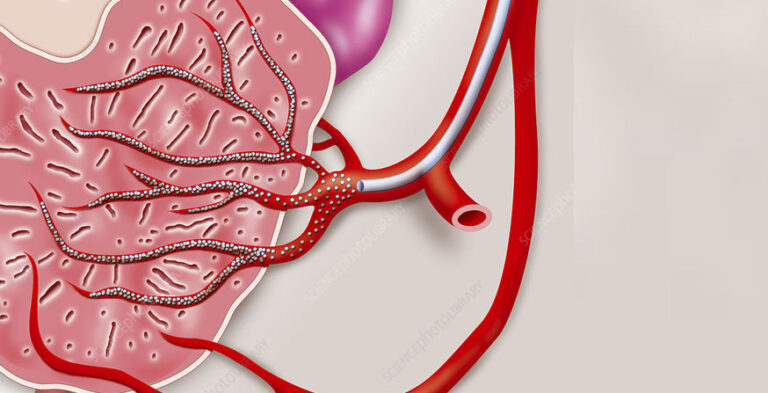
Prostate Artery Embolization is a relatively new, minimally invasive treatment for BPH. It involves selectively blocking blood flow to the enlarged prostate to reduce its size.
How PAE Works:
- Diagnosis: Before the procedure, patients typically undergo imaging tests, such as MRI or CT scans, to assess prostate size and the blood vessels supplying it.
- Procedure:
- An interventional radiologist accesses the femoral artery in the groin or radial artery in the wrist.
- A catheter is guided through the blood vessels to the prostate arteries using real-time imaging.
- Tiny particles are injected to block blood flow to the enlarged prostate, leading to its shrinkage over time.
- Recovery:
- PAE is usually performed on an outpatient basis, with patients going home the same day.
- Mild discomfort and bruising at the catheter insertion site may occur.
Benefits of PAE:
- Minimally Invasive: Requires only small incisions, leading to less pain and quicker recovery.
- Outpatient Procedure: Patients can return home the same day without the need for a hospital stay.
- Reduced Risk of Sexual Dysfunction: PAE has a lower incidence of erectile dysfunction and other sexual side effects compared to traditional surgery.
- Effective Symptom Relief: Studies show that PAE can reduce urinary symptoms and improve quality of life.
Risks of PAE:
Post-Embolization Syndrome: Some patients may experience flu-like symptoms in the days following the procedure.
- Infection: Although rare, there’s a small risk of infection at the catheter site.
- Urinary Complications: Some patients may experience temporary urinary retention or worsening symptoms.
Comparing Prostate Artery Embolization (PAE) and Traditional Surgery
When it comes to treating Benign Prostatic Hyperplasia (BPH), men have several options, including Prostate Artery Embolization (PAE) and traditional surgical procedures. Understanding the differences between these two approaches can help patients make informed decisions about their treatment. Here, we compare PAE and traditional surgery based on their mechanisms of action, invasiveness, recovery times, risks and complications, and overall effectiveness.
1. Mechanism of Action
Prostate Artery Embolization (PAE): PAE is a minimally invasive procedure designed to alleviate BPH symptoms by reducing blood flow to the prostate. The mechanism involves the selective blocking of the arteries that supply blood to the enlarged prostate. By injecting tiny particles into the prostate arteries through a catheter, the procedure decreases blood flow, leading to ischemia (reduced blood supply) in the prostate tissue. Over time, this ischemia causes the prostate to shrink, relieving pressure on the urethra and improving urinary symptoms.
Studies have shown that the effects of PAE can be gradual, with many patients experiencing noticeable symptom relief over weeks to months as the prostate reduces in size. Importantly, because the procedure targets the blood supply rather than removing tissue, there is less disruption to the surrounding anatomy, which can help preserve urinary and sexual function.
Traditional Surgery: In contrast, traditional surgical options for BPH, such as Transurethral Resection of the Prostate (TURP) and open prostatectomy, focus on the physical removal of excess prostate tissue. TURP involves the use of a resectoscope to cut away tissue through the urethra, while open prostatectomy requires a larger incision in the abdomen to remove tissue directly.
These surgeries aim to relieve urinary obstruction by removing the parts of the prostate that are causing pressure on the urethra. The immediate removal of obstructive tissue often leads to rapid symptom relief; however, this approach comes with more invasive implications, including a longer recovery time.
2. Invasiveness
Prostate Artery Embolization (PAE): One of the most significant advantages of PAE is its minimally invasive nature. The procedure is performed through small incisions, typically in the femoral artery (groin) or the radial artery (wrist). Using advanced imaging techniques, interventional radiologists can navigate the catheter to the prostate arteries with precision.
Because it is minimally invasive, PAE generally does not require general anesthesia and can often be performed as an outpatient procedure, allowing patients to return home the same day. The smaller incisions lead to less trauma to the body and a reduced risk of complications.
Traditional Surgery: Traditional surgical methods for BPH are significantly more invasive. Procedures such as TURP or open prostatectomy often require hospitalization and may involve general anesthesia. The surgical approach can lead to larger incisions, which, while effective, increase the potential for complications and longer recovery times.
Invasive surgeries can lead to longer hospital stays and increased postoperative care, as patients may need to manage pain, monitor for infections, and undergo rehabilitation. As such, patients may experience more discomfort and a prolonged adjustment period following traditional surgery.
3. Recovery Time
Prostate Artery Embolization (PAE): The recovery time associated with PAE is relatively quick. Most patients can resume normal activities within a few days following the procedure. Since PAE is less invasive, patients typically experience less postoperative pain and fewer complications, which contributes to a faster return to daily routines.
Patients may be advised to avoid heavy lifting and strenuous exercise for a short period post-procedure, but many find they can return to work and regular activities in a matter of days. Monitoring for symptoms and follow-up visits are typically scheduled a few weeks after the procedure to assess the effectiveness of treatment.
Traditional Surgery: In contrast, recovery from traditional surgical options can take weeks. Patients undergoing TURP or open prostatectomy may need to stay in the hospital for 1-3 days, depending on the procedure and individual recovery. The recovery process often includes managing pain, dealing with catheterization, and monitoring for potential complications such as bleeding or infection.
Postoperative care for traditional surgery can be extensive, as patients may experience side effects like urinary incontinence or sexual dysfunction, which can further prolong recovery and necessitate additional follow-up visits. Overall, the longer recovery period associated with traditional surgery can impact a patient’s quality of life and ability to engage in normal activities during their healing process.
4. Risks and Complications
Prostate Artery Embolization (PAE): PAE generally carries a lower risk of complications compared to traditional surgical options. Because the procedure is less invasive, the likelihood of serious complications such as bleeding or infection is reduced. However, PAE is not without risks.
Some patients may experience Post-Embolization Syndrome, characterized by flu-like symptoms, pelvic pain, or urinary frequency in the days following the procedure. This syndrome is typically self-limiting and resolves within a week. Although rare, there is also a potential for urinary retention or worsening urinary symptoms immediately after PAE.
Crucially, PAE has been shown to have a lower incidence of sexual dysfunction, making it an attractive option for many men concerned about preserving sexual health post-treatment.
Traditional Surgery: Invasive surgeries such as TURP and open prostatectomy come with a higher risk of complications. These risks include significant bleeding during or after the procedure, postoperative infections, and long-term issues such as urinary incontinence and erectile dysfunction.
Additionally, traditional surgeries can lead to retrograde ejaculation, where semen enters the bladder instead of exiting through the penis. This condition can affect fertility and is a concern for many patients.
While traditional surgical procedures have a long history of effectiveness, the risks associated with them can weigh heavily on a patient’s decision-making process, especially in terms of quality of life post-treatment.
5. Effectiveness
Prostate Artery Embolization (PAE): PAE has been shown to be effective for many patients, providing significant symptom relief and improving urinary flow. Clinical studies have reported that up to 80% of patients experience satisfactory improvement in symptoms after PAE. However, the effectiveness of PAE can vary based on prostate size and individual patient factors.
The gradual nature of symptom relief—often taking weeks to months—can be a drawback for some patients seeking immediate results. While PAE may not be suitable for all prostate sizes, particularly very large prostates, it remains a viable option for many men with moderate to severe symptoms.
Traditional Surgery: Traditional surgical options, especially TURP, have a proven track record of effectiveness, particularly for patients with significantly enlarged prostates. Many patients experience immediate improvement in urinary flow and a rapid reduction in symptoms.
Studies indicate that over 80% of patients report significant symptom relief following traditional surgical procedures. This immediate impact on symptoms can be a significant factor for patients who prioritize rapid results. However, the durability of symptom relief can vary, and some patients may experience recurrent symptoms over time.
Who is a Candidate for PAE?
While PAE is a promising treatment option, it is not suitable for everyone. Ideal candidates for PAE typically include:
- Men with moderate to severe BPH symptoms that significantly impact their quality of life.
- Patients who have not found relief from medications.
- Individuals seeking a minimally invasive treatment option with a reduced risk of complications.
Conversely, candidates for traditional surgery may include:
- Patients with severely enlarged prostates or those who have not responded to other treatments.
- Individuals who prefer a more aggressive approach to symptom relief.
- Patients who have significant urinary obstruction necessitating immediate intervention.
Consulting with Your Healthcare Provider
Deciding between Prostate Artery Embolization and traditional surgery requires careful consideration and consultation with a healthcare provider. Here are some factors to discuss:
- Severity of Symptoms: Your healthcare provider will evaluate the severity of your BPH symptoms and how they impact your daily life.
- Prostate Size: The size of your prostate can influence the choice of treatment. PAE may be more suitable for smaller prostates, while traditional surgery may be better for larger prostates.
- Overall Health: Your overall health, medical history, and any underlying conditions will affect treatment options and risks.
- Personal Preferences: Discuss your preferences regarding recovery time, potential risks, and desired outcomes.
Conclusion: Making the Right Choice for You
Prostate Artery Embolization and traditional surgery both offer viable solutions for managing symptoms of Benign Prostatic Hyperplasia. While PAE presents a minimally invasive alternative with a lower risk of complications, traditional surgical options have a proven track record of effectiveness.
Ultimately, the decision should be made collaboratively with your healthcare provider, considering your specific symptoms, prostate size, overall health, and personal preferences. Understanding the benefits and risks of each treatment will empower you to make an informed choice that aligns with your lifestyle and health goals.
By exploring these options, men suffering from BPH can take proactive steps toward reclaiming their urinary health and improving their quality of life.