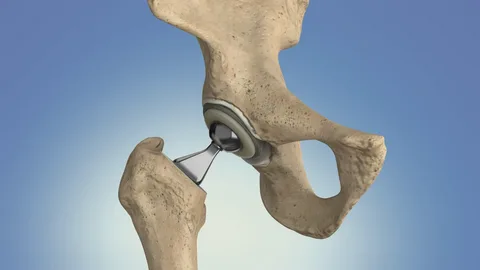
Total hip replacement (THR) is a highly successful surgical procedure designed to relieve pain and restore function in individuals suffering from hip joint issues. However, despite its effectiveness, some patients may require a revision total hip replacement (RTHR) due to various complications that arise over time. Understanding the common reasons for needing revision surgery is essential for both patients and healthcare providers. This blog will explore the ten most prevalent reasons for revision total hip replacement, shedding light on the complexities involved in maintaining hip health.
1.Aseptic Loosening
One of the most common reasons for revision surgery is aseptic loosening, where the implant becomes loose without any signs of infection. Over time, wear and tear can cause the bond between the implant and bone to weaken, leading to pain and instability. This condition is particularly prevalent in older implants or those subjected to high levels of activity, necessitating surgical intervention to restore stability.
2.Infection
Infection is a serious complication that can occur after a primary hip replacement. Bacteria may enter the joint space during surgery or from other parts of the body, leading to painful swelling and reduced function. When an infection is detected, it often requires revision surgery to remove the infected tissue and implant, followed by the placement of new components. Timely intervention is crucial to prevent further complications.
3.Recurrent Dislocation
Dislocation occurs when the ball of the hip joint comes out of its socket. This can happen if the components are not properly aligned or if surrounding muscles and ligaments are weakened. Multiple dislocations can damage the joint and increase the risk of further complications. Revision surgery may be necessary to correct alignment issues and stabilize the joint.
4.Periprosthetic Fracture
A periprosthetic fracture refers to a break in the bone surrounding the hip implant, often caused by trauma or weakened bone structure. These fractures can compromise the stability of the implant and may require revision surgery to repair the fracture and replace any damaged components. Addressing these fractures promptly is essential for restoring function and preventing further complications.
5.Implant Wear
All implants experience wear over time due to normal use, but certain factors—such as high activity levels or obesity—can accelerate this process. Wear particles can lead to osteolysis, where bone is resorbed around the implant, resulting in loosening and pain. When wear becomes significant, revision surgery may be necessary to replace worn-out components and restore joint function.
6.Osteolysis
Osteolysis refers to the gradual loss of bone around the implant caused by inflammatory reactions to wear particles released from the prosthesis. This condition can weaken bone structure and lead to implant loosening or failure. If osteolysis is detected, revision surgery may be required to address both the damaged bone and replace the affected implant components.
7.Component Failure
Although rare, component failure can occur when one or more parts of the hip implant break or become damaged due to excessive stress or manufacturing defects. This type of failure may necessitate revision surgery to replace broken components and restore proper function.
8.Joint Stiffness
Some patients experience stiffness in their hip joints after primary replacement surgery, which can limit mobility and quality of life. If conservative treatments such as physical therapy do not alleviate stiffness, revision surgery may be considered to address underlying issues contributing to limited range of motion.
9.Technical Errors During Initial Surgery
In some cases, technical errors during the initial surgery can lead to complications requiring revision. These errors might include improper alignment of components or inadequate fixation techniques that compromise joint stability. If identified early enough, corrective measures can be taken during a revision procedure.
10.Patient-Related Factors
Certain patient-related factors can significantly contribute to the need for revision surgeries following total hip replacements. Conditions such as obesity, diabetes, and osteoporosis complicate recovery and increase the risk of complications like infection or loosening of the implant over time. Addressing these underlying health issues before undergoing a primary or revision procedure is crucial for optimizing surgical outcomes.
Obesity is a prominent risk factor for complications after hip replacement surgery. Excess weight places additional stress on the hip joint and the surrounding structures, which can lead to premature wear of the implant. This increased load may result in loosening or failure of the prosthesis, necessitating revision surgery. Moreover, obesity is often associated with other health issues, such as diabetes, which can further complicate recovery. Patients who are overweight may also experience slower healing and a higher likelihood of infection, making preoperative weight management essential.
Diabetes is another significant factor that can impact surgical outcomes. It can impair wound healing and increase susceptibility to infections, both of which are critical concerns during and after hip replacement surgeries. Elevated blood sugar levels can hinder the body’s ability to fight infections and heal properly, increasing the chances of complications that may require revision surgery. Therefore, managing diabetes effectively prior to surgery is vital for ensuring better outcomes and reducing the risk of needing further interventions.
Osteoporosis, characterized by weakened bones, poses additional challenges for patients undergoing hip replacement. Patients with this condition have a higher risk of fractures and may struggle with bone integration around the implant. If the bone fails to adequately support the prosthesis, it can lead to loosening or instability over time. Addressing osteoporosis through medication or lifestyle changes before surgery can enhance bone density and improve the chances of a successful primary hip replacement.
In summary, patient-related factors such as obesity, diabetes, and osteoporosis can significantly influence the need for revision total hip replacement surgeries. By proactively addressing these underlying health issues before undergoing surgery, patients can optimize their surgical outcomes and reduce the likelihood of complications that may necessitate further interventions.
Revision total hip replacement is a complex procedure that may be necessary for various reasons following an initial hip replacement surgery. From aseptic loosening and infection to recurrent dislocation and component failure, understanding these common causes helps patients navigate their treatment options more effectively.
While undergoing a right hip total replacement surgery might seem daunting, advancements in surgical techniques have improved outcomes significantly, allowing many individuals to regain mobility and enhance their quality of life post-surgery. If you suspect that you may need a revision total hip replacement, consult with an experienced orthopedic surgeon who can provide personalized recommendations based on your specific circumstances.
By addressing these issues proactively, patients can take control of their hip health and work towards a more active, pain-free lifestyle in the long run.